
Potency answers a fundamental question:
Does the drug do what it’s designed to do?
Does the drug do what it’s designed to do?
Understanding potency testing in drug development
Potency testing is more than regulatory requirements. A properly executed potency assay provides a definitive measure of a drug's biological activity.
Today, a standardized, one-size-fits-all potency approach is insufficient in drug development. Developers need strategic, adaptable frameworks to meet regulatory and pipeline objectives, especially in a dynamic landscape, exemplified by complex modalities such as cell and gene therapies (CGTs).
This guide details why potency is a non-negotiable critical quality attribute in drug development. It highlights how a strategically designed potency assay determines the success of your drug candidate and ensures quality throughout the complete development pipeline.
What is potency?
Potency refers to the amount of a drug needed to achieve a specific biological activity; the "effect per dose." Drugs with high potency require lower doses to achieve a desired effect than those with low potency.
But in drug development, potency is far more than a simple effect-per-dose measurement. A drug's potency is a non-negotiable critical quality attribute that links its mechanism of action to its real-world clinical effect.
Understanding a drug candidate's potency answers a fundamental question in the development process: Does our product do what we designed it to do?
Addressing this question early can save drug developers significant time and effort.
Measuring potency in the drug development process ensures a drug's formulation is both stable and consistently functional. In fact, even slight variations between batches can significantly affect a drug's safety and efficacy.
Potency – a non-negotiable pillar in drug development
As we can see, potency testing extends beyond being a regulatory checkbox. It is a thread that fundamentally connects a drug's design in the lab to its real-world clinical functions. This highlights the significance of potency testing in drug development, a critical yet evolving requirement throughout a drug's path from discovery to commercial release.
Potency testing's significance in drug development can be divided into three imperatives:
1. The scientific and clinical imperative
A drug's potency reflects its biological activity, which results from its mechanism of action. Without a reliable measure of potency, there is no way to ensure that one batch of a drug will have the same therapeutic effect as another, ultimately affecting both patient safety and a drug's efficacy or, longer down the path, its effectiveness.
2. The commercial imperative
Consistency is also key to the successful commercialization of any drug. Even the slightest variations in potency between batches can undo years of research and development. Robust potency testing results in batch-to-batch consistency, drug stability, and ultimately, patient trust in the product.
3. The regulatory imperative
Given the high stakes, regulators such as the U.S. FDA and the European Medicines Agency (EMA) expect accurate potency data to demonstrate that a drug is clinically relevant, consistent, and high quality. These data are a key part of the marketing application's chemistry, manufacturing, and controls (CMC) section, which explains how the drug is made. If potency assays aren't up to standard, they undermine confidence in safety and efficacy. This can cause major setbacks, including regulatory delays or the failure to obtain regulatory approval. This is why developers need to be strategic and deliberate when selecting assays.
Potency at different stages of drug development
What does a typical drug development timeline look like, and where does potency testing fit?
Potency testing strategies differ depending on the type of drug, with no clear blueprint. Importantly, the approach for potency assessment evolves as the drug progresses from early screening to lot release, with each stage of the drug's regulatory path presenting unique challenges and solutions. This dynamic underscores the importance of selecting the right assay from the get-go.
The path from early to late stages shifts priorities:
- Early-stage assays: prioritize speed and adaptability to characterize the biological function, connect it to the mechanism of action, and select a candidate quickly.
- Late-stage assays: require stringent regulatory standards (e.g., ICH Q6B for biologics and specialized regulatory guidelines) for batch release, stability testing, and biosimilar comparability, especially for complex modalities such as CGTs.
As intentions and approaches to potency testing change across the development process, so do the distinct obstacles at each stage. Beyond aligning assays with complex mechanisms of action, developers must also establish and maintain optimal, stable reference standards.
How, then, do you address priorities and challenges of potency testing throughout the drug development pipeline?

Requirements vary across development stages, each presenting unique challenges
Potency assays in early drug development
Balancing speed and scientific accuracy
Early drug development, such as discovery, preclinical, and early clinical studies, focuses on identifying promising candidates and demonstrating proof of concept.
Priorities
This stage prioritizes fast candidate characterization and adaptable study designs that yield reliable, repeatable data. Here, developers balance speed and scientific accuracy, even when working with complex biological systems.
Objectives
Identify promising candidates using streamlined fit-for-purpose potency assays. A well-planned strategy can smooth the transition from early development to later phases and minimize the risk of regulatory delays.
Approach
At this stage, developers choose assays depending on the therapeutic modality. The overarching goal is to get quick yet functionally reliable answers: Does it bind (target engagement)? Does it work (biological activity)? How strong is it (dose-response)? Strategies differ depending on the drug candidate. For example, enzyme binding assays can be used to assess small molecules, while functional cell-based systems are ideal for biologics. Achieving a robust understanding of the drug candidate's performance requires qualified protocols, often with pre-configured yet flexible off-the-shelf formats.
Potency assays in late-stage development
Complying with strict regulatory guidelines
As the development process reaches late-stage and regulatory submissions, expectations rise, and regulators require strict adherence to quality guidelines.
Priorities
Later stages require compliance with international quality standards, such as the ICH Q6A and Q6B, which safeguard the consistency, safety, and efficacy of a drug. While Q6A highlights quality standards for new drug substances and products, including small molecules, Q6B applies to biotechnological and biological products.
Objectives
Potency analysis and assays used at this stage show that a drug's function and mechanism of action meet standards for stability, comparability, and lot release. Potency testing during these late stages provides the evidence needed for market authorization or approval.
Approach
Meeting the rigorous standards of late-stage development requires that developers tailor their strategies to yield a more comprehensive understanding of the drug candidate's function. Custom assays are often the go-to approach for validating a candidate's critical function. For example, using orthogonal methods (multiple experimental methods) or other complementary approaches helps generate robust datasets and proactively prevents misaligned outcomes that delay results.
How to measure potency
The "how" of potency testing is dictated by the modality. While the significance and imperatives of potency testing apply to all therapeutic categories, the specific strategies and assay methods differ between small molecules and biologics.
Small molecules
Because small molecules often act through well-defined, single-target mechanisms, verifying potency typically focuses on measuring substrate binding or enzymatic inhibition. This biochemical approach is effective because the drug's activity is directly tied to a single, quantifiable interaction. When testing the potency of small molecules, laboratories usually quantify the concentration that inhibits a target enzyme by 50% (IC50) or the concentration that produces 50% of the maximum effect (EC50). Researchers typically generate data for IC₅₀ or EC₅₀ calculations using techniques such as enzyme activity assays, high-throughput screening, and, increasingly common, fluorescence polarization.
Biologics
The requirements for biologics, such as monoclonal antibodies and CGTs, are more stringent than for small molecules. Their biology often involves complex interactions, for which straightforward biochemical measurements are insufficient.
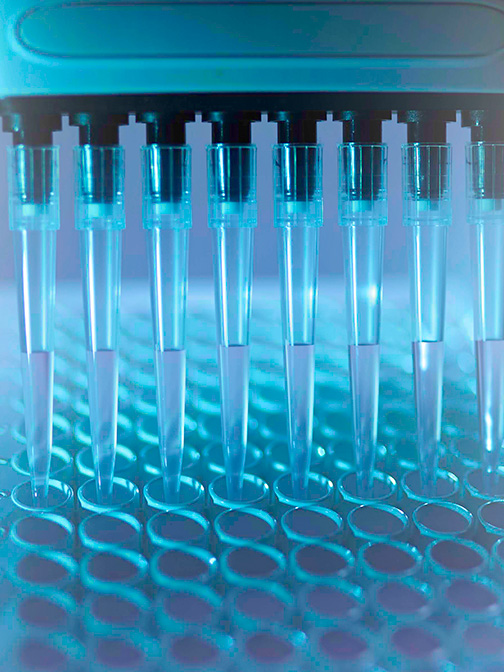
Measuring the potency of these more complex therapeutics requires tailored functional bioassays that reflect their mechanisms of action (MoA), such as blocking a receptor or neutralizing a ligand. Because of their inherent complexity, potency assays for biologics must measure therapeutic responses beyond what simple biochemical interactions can reveal. As a result, developers testing these modalities increasingly rely on cell-based assays, tests that measure biological activity in living cells.
Tailored strategies for evolving opportunities
With the emergence of new biotechnologies and growing global collaborations between experts, the drug development field is constantly introduced to therapeutic innovations. Although these advancements offer unprecedented benefits in clinics worldwide, their variety and pace of development also introduce new pipeline challenges.
Adding to this complexity, each modality requires evolving approaches as it progresses through the drug development stages to ultimately reach patients.
A standardized one-size-fits-all potency approach is insufficient in today's dynamic drug development landscape. Instead, developers need adaptable, customizable strategies to streamline the development process. But what does overcoming these specific challenges look like in practice?
Tailored, multi-faceted strategies consider the unique properties of specific modalities and their evolving requirements. Fortunately, the biotechnological field evolves alongside these constantly increasing demands. From pre-configured, off-the-shelf potency assays in the early stages to customized orthogonal methods used later in the process, more refined approaches are continually being developed.
These strategies support developers throughout the pipeline, saving time, effort, and resources. Most importantly, they lead to consistent, stable, effective, and safe products. This ultimately builds patient trust in the therapies, and, by extension, in the developers behind them.
